2 Minute Medicine Rewind May 20, 2024
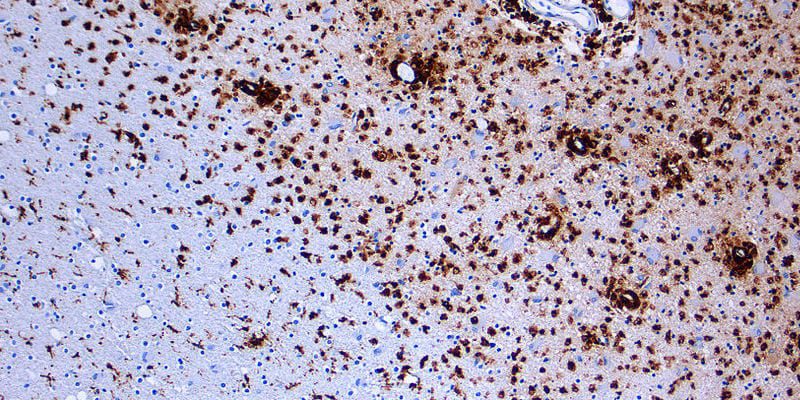
Temporal Relationship Between Serum Neurofilament Light Chain and Radiologic Disease Activity in Patients With Multiple Sclerosis
1. Serum neurofilament light chain (sNfL) elevations are a relatively specific biomarker of magnetic resonance imaging (MRI) disease activity in multiple sclerosis (MS) (82%–91.9% specificity) but have a low sensitivity (27.9%–42.6% sensitivity )
2. Peak increase in sNfL was observed at an average of 9 weeks after the first Gd+ lesion was seen and remaining high after resolution of Gd+ lesions in many participants.
Evidence Rating Level: 1 (Excellent)
Magnetic resonance imaging (MRIs) have been validated and included in the international guidelines for use as a prognostic marker in multiple sclerosis (MS). Due to the cost of MRI, a blood-based biomarker for inflammatory activity is needed to monitor disease progression and guide treatment. Neurofilament is a component of neuron cytoskeleton and serum neurofilament light chain (sNfL) levels correlate with disease activity, may predict prognosis, and are reduced by treatments. However, the interpretation of sNfL is currently limited by a lack of understanding of the temporal relationship between sNfL levels and disease activity. Researchers sought to further assess this in this post-hoc analysis of the RESTORE randomized trial, by comparing patients undergoing interruption natalizumab therapy and those that remained on the therapy for 24 weeks. Monthly serum and MRIs were taken to correlate MRI disease activity (ie, gadolinium-enhancing lesions) and serum biomarkers. Compared to those without gadolinium-enhancing lesions (Gd+ lesions), participants with Gd+ lesions had significantly higher sNfL mean levels at 28 weeks (20.0 ± 30.5 vs 10.2 ± 7.9 pg/mL; p = 0.004). From baseline to week 28, participants who developed Gd+ lesions had a mean ± SD percentage increase in sNfL of 126.6% ± 232.2% vs 8.9% ± 46.2% (p < 0.001) in the participants who did not develop Gd+ lesions. There was also an increase in baseline and peak sNfL as the number of Gd+ lesions increased. In 80% of participants, new Gd+ lesions appeared before any increases in sNfL levels whereas 20% of patients reached peak sNfL levels before new Gd+ lesions were identified. Peak sNfL was delayed by an average of 8.7 ± 14.4 weeks after the first Gd+ lesion identification. Most patients with Gd+ lesions did not have elevations in sNfL levels. Using the 95th percentile sNfL levels of participants without Gd+ lesions as a threshold, sNfL was determined to be a relatively specific biomarker of MRI disease activity in MS (82%–91.9% specificity) but had low sensitivity (27.9%–42.6% sensitivity) . Further research into this domain may provide more insight into the possible role of sNfL as a prognostic biomarker for MS.
Gender differences in PTSD severity and pain outcomes: Baseline results from the LAMP trial
1. Post-traumatic stress disorder (PTSD) symptoms were associated with higher levels of chronic pain, pain catastrophizing, and pain interference among US veterans.
2. No significant gender differences were found in the associations between PTSD symptoms and pain outcomes.
Evidence Rating Level: 2 (Good)
Post-traumatic stress disorder (PTSD) and chronic pain are highly prevalent comorbid conditions in both veterans and civilians. Patients dually burdened by both PTSD and chronic pain experience more severe psychiatric impairments and incur a greater cost to the healthcare system. Few studies have enrolled enough women to test the gender difference in pain outcomes (pain catastrophizing, interference, and intensity) relative to PTSD symptoms. In this secondary analysis of a randomized clinical trial, a linear regression model was used to analyze 421 men and 386 women Veterans with chronic pain who provided complete data on PTSD symptoms and pain outcomes. PTSD symptoms were associated with higher levels of pain catastrophizing (0.57, 95% CI [0.51, 0.63]), pain intensity (0.30, 95% CI [0.24, 0.37]), and pain interference (0.46, 95% CI [0.39, 0.52]). Gender differences were not found using crude models or those adjusted for sociodemographic characteristics (all interaction p-values<0.05). While women Veterans had higher average PTSD symptom cores, pain catastrophizing, pain intensity, and pain interference, no significant differences were present in interaction models between PTSD and chronic pain. Differences could be minimized due to the strict inclusion criteria which could skew participants to be more similar than the true veteran population. Overall, study findings suggest a correlative relationship between PTSD symptoms and both the sensation and cognitive processing of pain, with no sex-related differences observed.
Humeral Component Version Has No Effect on Outcomes Following Reverse Total Shoulder Arthroplasty A Prospective, Double-Blinded, Randomized Controlled Trial
1. Neutral version and 30° retroversion humeral components in reverse total shoulder arthroplasty had no significant difference in range of motion, muscle strength, or patient-reported outcomes.
Evidence Rating Level: 1 (Excellent)
Reverse total shoulder arthroplasty (rTSA) for patients with rotator cuff tear arthropathy improves forward elevation, pain, and function but can result in limited internal and external rotation. The goal of this randomized control trial was to determine if internal and external rotation are affected by the positioning of the humeral component (neutral or 30° of retroversion). Patients were stratified in a 1:1 ratio using a computer-generated randomized sequence and surgeons were informed of decisions just before surgery by non-data collecting personnel. Baseline data was collected before surgery and follow-up data was collected 3 months, 1 year, and 2 years postoperatively. Patients were given a patient-reported outcomes questionnaire and underwent a physical examination by a coordinator blinded to the study groups. Shoulder range of motion was measured using a goniometer, strength was measured using an isometer, and radiographs were obtained at each visit. Both neutral version and retroversion saw significant improvements in forward (97.3° to 139.1°and 94.0° to 132.2° respectively, p<0.001 in both groups). Similarly, active abduction improved significantly in both neutral version and retroversion groups (94.9° to 134.9°, p<0.002; and 86.2° to 128.6°, p<0.001 respectively). Neither group saw a significant increase in active internal or external rotation. Patient-reported outcomes also showed significant improvement overall but no differences between groups. Finally, both groups showed significant improvement in strength in forward elevation, abduction, and external rotation. Only the retroversion group showed a significant improvement in internal rotation strength. Overall, no significant differences were noted between the two groups.
Effect of Endovascular Thrombectomy for Acute Ischemic Stroke on Cognitive Outcomes A Secondary Analysis of the ESCAPE Trial
1. In post-stroke patients, endovascular thrombectomy (EVT) was associated with favorable outcomes on 5 separate cognitive tests that showed benefits to global cognitive function.
Evidence Rating Level: 2 (Good)
Endovascular thrombectomy (EVT) is a highly effective treatment for large vessel occlusion strokes that can improve functional neurological outcomes. While EVT reduces infarct volume, cognitive outcomes have not been well-studied. To validate the quality of EVT therapy, patients were randomized to be treated either with the standard medical therapy or with standard medical therapy and EVT. To assess global cognitive outcome, five separate tests were administered 90 days after stroke: the Montreal Cognitive Assessment (MoCA), the Sunnybrook Neglect Assessment Procedure (SNAP), the Boston Naming Test (BNT), Trail-making test A (Trails A) , and Trail-making test B (Trails B). EVT resulted in significantly better performance on all five cognitive tests. EVT was significantly lowered final infarct volume (FIV) which was significantly associated with higher cognitive performance. Even when FIV is controlled for, EVT showed greater cognitive function. Longer-term outcome studies are needed to assess the effect of EVT on post-stroke dementia which can appear in 8.2-34% after 1 year depending on stroke severity.
Bone mineral density and related clinical and laboratory factors in peritoneal dialysis patients: Implications for bone health management
1. In patients undergoing peritoneal dialysis, osteoporosis is highly prevalent but does not correlate to 25-vitamin D levels.
Evidence Rating Level: 3 (Average)
One complication in patients with chronic kidney disease (CKD is increased bone turnover and decreased bone density. Bone mineral density (BMD) indicates bone mass and mineralization. It is determined using a Dual-Energy X-ray Absorptiometry (DEXA) scan at both the posteroanterior lumber spine (L1-L4) and the hip (femoral neck or total proximal femur). Previous meta-analysis highlighted the significant relationship between a CKD and a low BMD which increases their fracture risk. Currently, there is conflicting evidence regarding DEXA scan measurements and biochemical markers of osteopenia and osteoporosis. In this cross-sectional study, researchers aimed to determine the prevalence of in patients undergoing peritoneal dialysis (PD) and to correlate the associated biochemical variables. Patients undergoing PD were evaluated for clinical characteristics, biochemical markers , and BMD. Vitamin D investigations showed 86.8% of participants had a deficiency with a median of 8.7ng/mL. BMD measurements revealed an osteoporosis rate of 41% in the femoral neck and 38% in the lumbar spine. A multivariate analysis attempting to correlate 25-vitamin D levels with BMD showed no significant correlation. However, another multivariate analysis showed BMI had a positive correlation with BMD in both the femoral neck and lumbar spine. More investigations into clinical and biochemical markers of osteoporosis in PD patients are needed to begin osteoporosis treatment promptly. Vitamin D supplementation should be considered prophylactically in PD patients.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

Ethel Purdy – Medical Blogger & Pharmacist
Bridging the world of wellness and science, Ethel Purdy is a professional voice in healthcare with a passion for sharing knowledge. At 36, she stands at the confluence of medical expertise and the written word, holding a pharmacy degree acquired under the rigorous education systems of Germany and Estonia.
Her pursuit of medicine was fueled by a desire to understand the intricacies of human health and to contribute to the community’s understanding of it. Transitioning seamlessly into the realm of blogging, Ethel has found a platform to demystify complex medical concepts for the everyday reader.
Ethel’s commitment to the world of medicine extends beyond her professional life into a personal commitment to health and wellness. Her hobbies reflect this dedication, often involving research on the latest medical advances, participating in wellness communities, and exploring the vast and varied dimensions of health.
Join Ethel as she distills her pharmaceutical knowledge into accessible wisdom, fostering an environment where science meets lifestyle and everyone is invited to learn. Whether you’re looking for insights into the latest health trends or trustworthy medical advice, Ethel’s blog is your gateway to the nexus of healthcare and daily living.