
Let go of stress! How trauma arises and disappears
The diagnosis and number of mental illnesses and disorders are increasing rapidly. New findings on the origin and development of stress-related illnesses such as trauma or depression are opening up new avenues for diagnosis and individual treatment.
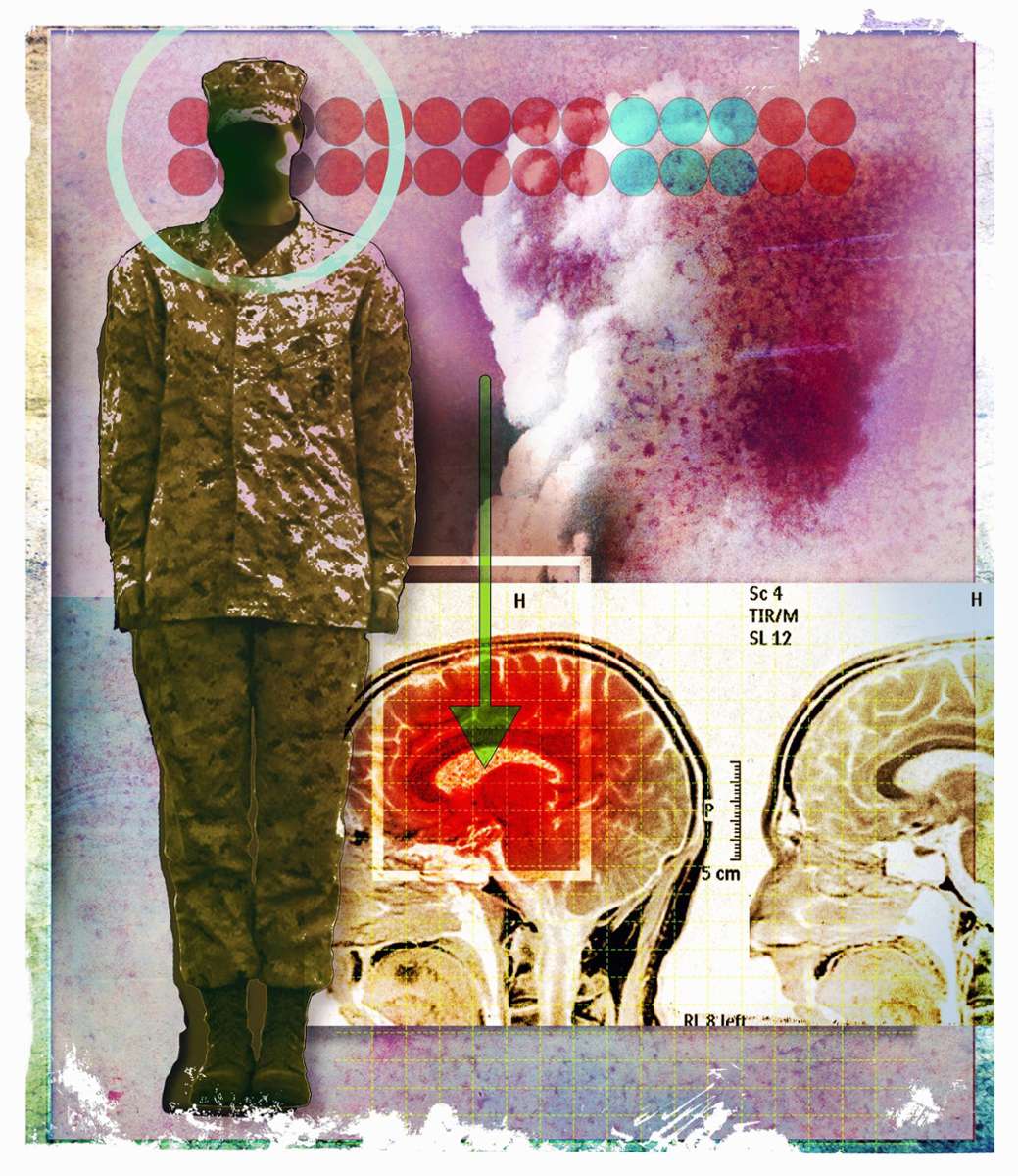
Experiencing or witnessing a traumatic event – such as a serious accident, a natural disaster, the loss of a loved one, or war and violence – can cause great psychological damage. The symptoms of this post-traumatic stress disorder (PTSD) can appear immediately after the traumatic event or begin months or even years later and can significantly affect daily life.
Eight percent of people worldwide suffer from PTSD
Around eight percent of all people suffer from PTSD over the course of their lives, with women being affected more often than men. However, there is a good chance of recovery. “The sooner PTSD is treated professionally with psychotherapy, the greater the likelihood of being able to return to normal everyday life,” says Jürgen Deckert, Director of the Clinic and Polyclinic for Psychiatry, Psychosomatics and Psychotherapy at the University Hospital of Würzburg.

In a new study, Deckert and a team of researchers investigated how to better understand the neurobiological basis of PTSD and open up avenues for new treatment options. In the study published in the journal Nature Genetics, the scientists analyzed the genetic characteristics of PTSD.
“Predisposition factors can make people more resilient or more vulnerable to extreme experiences,” explains Deckert. “Not everyone develops post-traumatic stress disorder after a traumatic event.”
Certain genes increase the risk of developing PTSD
For their study, the researchers examined the data of more than 1.2 million people. Of the 95 genetic regions discovered that are linked to PTSD, 80 were previously unknown. “When we examined these genetic regions more closely, we identified 43 genes that increase the risk of developing post-traumatic stress disorder after a trauma,” reports biologist Heike Weber from the Center for Mental Health (ZEP) at the University of Würzburg.

According to the researcher, these 43 newly identified genes are mainly responsible for the regulation of nerve cells and synapses, brain development, the structure and function of synapses, and hormonal and immunological processes. Other important genes influence stress, anxiety, and threat processes, which are believed to underlie the neurobiology of PTSD. For info: A synapse is a contact structure for the transmission of a chemical or electrical signal from one nerve cell to another nerve cell or another target cell (muscle cell, gland cell, sensory cell).
Biochemical causes of PTSD and depression
A second study, which builds on the publication in “Nature Genetics”, has been published in the journal “Science”. This study looks at the molecular and biochemical causes of PTSD and depression.
Both stress-related mental disorders arise from the interaction of genetic susceptibility and stress, which gradually lead to changes in the human genome (all the genetic information present in a cell). This in turn affects the interaction between genes and proteins.
To find a connection between PTSD and depression, the researchers of the “Science” study supplemented data from examinations of various brain regions with analyses of so-called single-nucleus RNA sequencing (which provides detailed insights into the state and activity of individual cells), genetics and proteomics of blood plasma. For info: Proteomics is a biochemical procedure to study the totality of all proteins present in a cell or living organism and their properties.
New therapies to detect disease signals early
The researchers found most of the disease signals in the medial prefrontal cortex. The prefrontal cortex is part of the frontal lobe of the cerebral cortex and is located at the front of the brain. These signals affect the immune system as well as the regulation of nerve cells and stress hormones.
The combination of both studies shows that there are common and different molecular disorders in the brain in both PTSD and depression, in which specific cell types are involved. If these connections are investigated further, the scientists say, stress-related signaling pathways could be derived that could provide clues to new therapeutic approaches for both diseases.
These new approaches could complement and expand existing therapies. You can find out what these are in the following info read more.
Info: The traumatized soul
Psycho-traumatology
Psychotraumatology deals with the consequences of trauma, researching and treating the effects of traumatic events on the experience and behavior of individuals and groups. The term “traumatology”, which originates from accident surgery, was applied to psychological injuries by the American child psychiatrist Dennis Donovan in 1990. This gave rise to the concept of psychotraumatology.
PTSD
The fact that people cannot simply process experiences of violence, separation, abuse or war ad hoc leads to so-called post-traumatic stress disorder (PTSD) – that is, lingering psychological stress. Although this phenomenon has been known for a long time, PTSD has only been diagnosed since 1980 in connection with dissociative disorders (where related information, perceptions or thoughts can no longer be linked to one another) with its inclusion in the DSM.
DSM/ICD
The DSM (Diagnostic and Statistical Manual of Mental Disorders) is a diagnostic and statistical guide to mental disorders. It has been published by the American Psychiatric Association since 1952 and has been published in German since 1996. The DSM-5 plays a central role in the definition and diagnosis of mental illnesses. Today, the DSM is used internationally in research and in many clinics and institutes. The ICD (International Statistical Classification of Diseases and Related Health Problems) is the second major classification system in medicine. It includes the International Statistical Classification of Diseases and Related Health Problems and is the most important, globally recognized classification system for coding diagnoses in outpatient and inpatient medical care. It is published by the World Health Organization (WHO).
Psychological therapies for PTSD
Depth psychology
Depth psychology is used to look for the effects of trauma on the subconscious. In 100 or more individual sessions, deeply hidden and repressed experiences are brought to light, addressed and processed.
Imaginative procedures
In this process, deeper layers of the soul, which are hidden in everyday life, are brought to the surface through inner images and dreams. This should ultimately lead to a psychologically conscious and deeper level of processing.
Narrative procedures
The idea here is that traumatized people can live out their inner urge to recount lost, isolated or repressed traumas. By describing (narrating) the personal life story, one tries to find meaning and connection in the experiences.
Gestalt therapy
Gestalt therapy is a psychotherapeutic method that allows the body, mind and soul to participate in the processing of trauma in a holistic (integrative) way. All three levels, as well as the social environment of the person affected, influence each other and must be taken into account in therapy, for example in body therapy methods such as art therapy. The hands are used for painting, shaping and designing and thus become instruments for the mental and emotional processing of trauma.
Medication
Certain illnesses lead to psychological symptoms such as phobias, panic attacks or depression, which can only be treated with the help of special medications (such as tranquilizers, antidepressants or neuroleptics). However, it is controversial whether such medications are the right approach for trauma patients – also because they do not address the causes of the stress disorders.

Ethel Purdy – Medical Blogger & Pharmacist
Bridging the world of wellness and science, Ethel Purdy is a professional voice in healthcare with a passion for sharing knowledge. At 36, she stands at the confluence of medical expertise and the written word, holding a pharmacy degree acquired under the rigorous education systems of Germany and Estonia.
Her pursuit of medicine was fueled by a desire to understand the intricacies of human health and to contribute to the community’s understanding of it. Transitioning seamlessly into the realm of blogging, Ethel has found a platform to demystify complex medical concepts for the everyday reader.
Ethel’s commitment to the world of medicine extends beyond her professional life into a personal commitment to health and wellness. Her hobbies reflect this dedication, often involving research on the latest medical advances, participating in wellness communities, and exploring the vast and varied dimensions of health.
Join Ethel as she distills her pharmaceutical knowledge into accessible wisdom, fostering an environment where science meets lifestyle and everyone is invited to learn. Whether you’re looking for insights into the latest health trends or trustworthy medical advice, Ethel’s blog is your gateway to the nexus of healthcare and daily living.



